Kefir: A Potent Immune-Enhancing Fermented Food with Promising Cancer Prevention Properties

Kefir is a fermented beverage, usually made from dairy, that has beneficial health effects due to its antioxidant, antimicrobial, and anti-inflammatory properties.1 Kefir originates from the Caucasus region (between the Black Sea and Caspian Sea), and from Tibet (between China and India). Research also suggests its probiotic content directly influences the immune system’s cancer surveillance capabilities. Recent research […]
Nutritional Impact on Immunity and COVID – 19
Although statistics show that people over the age of 65 have an increased risk of contracting COVID-19 and dying from complications due to underlying conditions, it appears that it has more to do with nutritional status than age alone. It’s true that the older we get, the more nutritional deficiencies we may have, primarily because […]
There’s No Substitute for Sunlight: The Essential Influence of Nature’s Sunshine Vitamin on Health
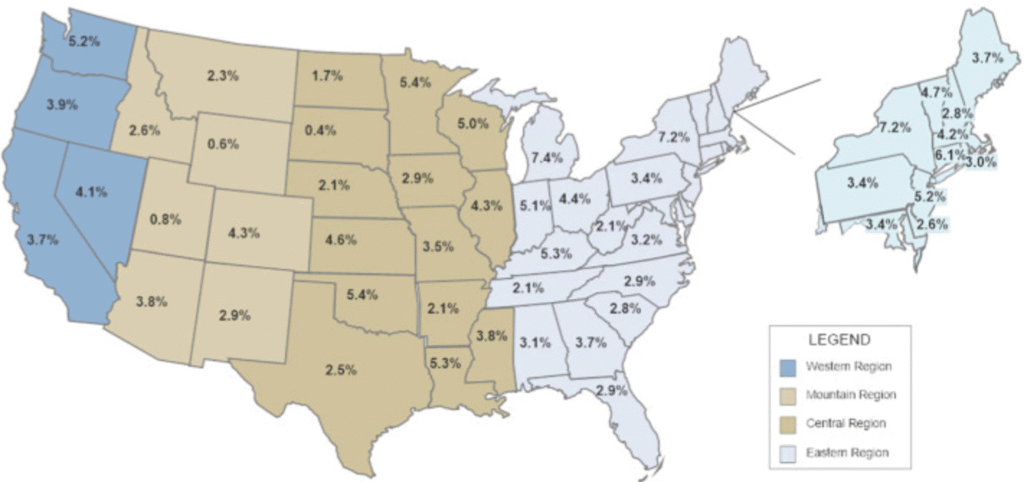
The distribution of community outbreaks of the current global pandemic shows seasonal patterns associated with latitude, temperature, and humidity, which is similar to the behavior of seasonal viral respiratory tract infections.[1] The seasonality of many viral infections is associated with a lack of sunlight, which results in low 25(OH)D concentrations and an uptick in diseases […]
Understanding Neutrophil to Lymphocyte Ratio: The Most Important and Overlooked Biomarker of Systemic Inflammation in Cancer: Part 1

Inflammation is an essential part of our body’s immune defense. When we encounter pathogens such as bacteria, viruses, or parasites, our body responds with inflammation to fight the invaders and increase immune response. In these instances, inflammation is beneficial. But inflammation has a dark side—left unchecked, it can wreak havoc on cells, tissues, and organs. […]
Holy Basil: An Herb With Incomparable Benefits

Closely related to the culinary herb sweet basil (Ocimum basilicum), holy basil (Ocimum sanctum) is a plant with a rich history of use as a healing herb. Because this venerable herb has so many applications, it has become one of my favorites. I often include holy basil in adaptogenic tonics, and also find it useful […]
An Herbal Approach To Rheumatoid Arthritis

I recently conferred with a patient who had been diagnosed with rheumatoid arthritis (RA), a chronic inflammatory type of arthritis that affects the lining of the joints, causing painful swelling and potential joint destruction and deformity. The standard treatment for the disease is high dosages of pharmaceutical drugs, including anti-inflammatories, steroids, and immune suppressive drugs. […]
Can Statins Be Avoided With Lifestyle Interventions? Part 2

In part 1 of this series, I provided an in-depth evaluation of the powerful role that diet plays in cardiovascular health, particularly in regard to achieving healthy cholesterol levels. As I pointed out in that post, I do not recommend statins, except in rare cases. Even then, the dosages I recommend are far less than […]
Thoughts on Healthy Aging

This may seem to be a radical stance, but I believe it is mistake to think that illness and disease are an inevitable part of the normal aging process. Although we may think of aging in relation to outward appearance, the way we look reflects only certain aspects of age, some of which are superficial–such […]
Fish Oil Supplements: Beneficial Or Not?

If you believe the findings of a recent highly publicized research report, you may be wondering if you should throw your fish oil supplements into the garbage. According to a study published in the Journal of the American Medical Association (September 2012), researchers who evaluated data from 20 previous studies maintain that neither fish oil […]
