Have you heard some buzz about oxalates in spinach and other leafy vegetables? A theory that’s been gaining popularity among those interested in nutrition is that we should avoid greens, especially spinach, because they are high in oxalates. After all, oxalates can cause kidney stones or gallbladder problems and may interfere with calcium absorption.
So, one of the latest and greatest trendy dietary recommendations is to STOP eating foods high in oxalates, especially for people with oxalate sensitivity. As a result, spinach, kale, and many green oxalate-containing foods have become public enemy number one! Should you take heed? Is it time to eliminate leafy greens from your healthy diet because of the oxalates in spinach? The short answer to this question is a resounding “NO!”. But, let’s check out why.
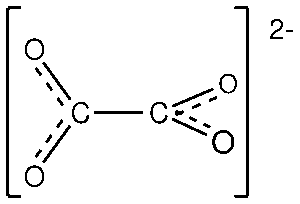
What’s an Oxalate?
Oxalic acid is a common organic compound that occurs naturally in plants and humans. Oxalates are highly reactive. They’re attracted to positively charged minerals, such as calcium and iron, and like to form calcium oxalate and iron oxalate.
In plants, oxalic acid helps to eliminate extra calcium from the plant. When a plant has an infection, oxalic acid can quench calcium ions released during cell wall breakdown to protect against toxic calcium concentrations in the infection area. Oxalic acid plays a detoxifying role during the late infection stages.[1]
Various living organisms produce oxalic acid, including fungi, bacteria, plants, animals, and humans. This is why many plants are high in oxalates.
However, there are many reasons you may have an oxalate issue or be reacting to higher oxalates in spinach and other foods.[2]
The Truth About Dietary Oxalates
When we consume oxalate-rich foods, oxalates travel through our digestive tract, binding with calcium. The beneficial intestinal microbiota easily consumes these sharp tiny bound crystals, eliminating them via our stool.
Oxalate consumption usually is not an issue. However, sometimes the digestive tract is already inflamed from food allergies or damaged due to a leaky gut or the presence of chemicals. Refined and processed foods, glyphosate, antibiotics, and even stress can all disrupt the microbiome and damage the digestive tract. Then you may start having issues with oxalates in spinach.[3]
Gut Health and Oxalates
Gastrointestinal microbiota plays a role in oxalate metabolism, one of the significant proportions of nephrolithiasis, possibly by affecting the intestinal absorption of oxalate and renal stone formation.
Microbiota manipulation prevents oxalate kidney stone formation. Diverse gut bacteria are essential, but Bifidobacterium (yogurt and kefir) specifically possess oxalate-degrading abilities.[4],[5] This prevents it from binding to minerals and affecting nutrient absorption. Oxalobacter and Lactobacillus species exist symbiotically in the human gut and prevent stone formation by altering some biochemical pathways through the production of specific enzymes, which help in the degradation of oxalate salts. Synbiotic supplementation has a beneficial effect on the total oxalate-degrading activity of gut microbiota.[6],[7]
Peer-reviewed research reveals that the ability of oxalates to lower calcium absorption is small and does not outweigh the power of those foods to contribute significant calcium to the diet. Spinach is rich in calcium. Research does not support the notice that restricting spinach in the diet reduces the risk of stone formation.[8]
Dietary principles and recommendations for oxalate prevention include adequate fluid intake, modest calcium intake, low dietary sodium, magnesium, potassium, and limited animal protein.[9]
What About Sugar?
On the other hand, sugar—specifically in the form of refined fructose like corn syrup—is very bad for gut health. One study showed that consuming one sugar-sweetened soda daily was associated with a 23–33% greater risk of stone formation than consuming less than one weekly serving.[10] Fructose increases urinary stone formation and may contribute to kidney stone development, especially in people with metabolic disorders and those suffering from heat stress.[11]
Eat These Foods to Alkalize and Support Kidney Health and Oxalate Excretion:
- soy, such as miso, soybeans, tofu, and tempeh
- whole milk yogurt (Sheep, goat, or cow)
- most fresh vegetables, including potatoes
- most fruits – figs in particular, and fresh citrus fruit – but not commercial fruit juices
- herbs and spices, excluding salt, mustard, and nutmeg
- beans and lentils
- some whole grains, such as millet, quinoa, and amaranth
- herbal teas
- fats like olive oil, avocados, nuts, and seeds
- Apple cider vinegar
Citrus (lemons, oranges, grapefruit, and lime) and non-citrus fruits (melon) are natural sources of dietary citrate. Several studies have shown the potential of these fruits in raising urine citrate levels. Lemons are a specific inhibitor of oxalates.[12] Citrate acts as an inhibitor of calcium oxalate and calcium phosphate stone formation.[13],[14]
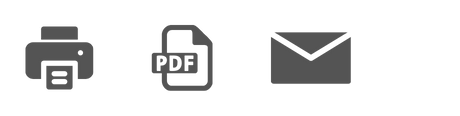
Parsley is a treatment for various renal diseases. Its benefits could be due to its bioactive constituents, including flavonoids (apigenin), carotenoids, coumarins, tocopherol, and ascorbic acid. The high content of chlorophyll and magnesium and parsley’s alkalizing effects are also a reason for its inhibitory effect of calcium oxalate.[15]
Magnesium forms a complex with oxalate and decreases it, which can reduce the risk of stone formation. Magnesium can also bind with oxalate in the gastrointestinal tract to reduce oxalate absorption.[18],[19]
A Healthy Whole Food Diet
So, to avoid kidney stones, you need to eat a healthy and balanced diet of whole foods which offer an array of health-promoting compounds.
Daily oxalate intake of 40-50 mg. has no impact on causing oxalate kidney stones.[20]
Your body makes oxalates in the liver. The mean daily intake of oxalate in English diets has been calculated to be 70-150 mg, with tea appearing to contribute the most significant proportion of oxalate in these diets; rhubarb, spinach, and beets are other common high oxalate-content foods.[21]
Of note, no published study has demonstrated a significant benefit of dietary oxalate restriction on actual stone recurrence.[22] The key is not avoiding dietary oxalates but eating them in moderation as part of a healthy balanced diet.
Despite Oxalates in Spinach, Spinacia Oleracea Has Many Health Benefits
Spinach is rich in vitamins and minerals.[23] It has neuroprotective,[24] [25] antihyperlipidemic,[26] antiglycation,[27] appetite suppressive,[28] anti-osteoarthritic,[29] hepatoprotective,[30] antioxidant,[31] antitumor, antiproliferative, and anti-inflammatory properties.[32]
Spinach contains flavonols, polyphenols, and vitamins (A, B1, B2, B3, B6, C, E, K, and folic acid).
This wide array of antioxidant phytoconstituents in spinach renders it a potent ROS scavenger and antioxidant.[33]
The chemical composition of spinach includes carotenoids, the phenolic compounds quercetin and kaempferol, derivatives of patulin, spinacetin, spinatoside, jaseidin, and flavone, as well as various phenolic acids, primarily ferulic and p-coumaric acid.
Several studies have found that spinach inhibits colon tumor growth[34] and that spinach compounds suppress colon cancer.[35] Other science has shown that spinach extract enhances the cytotoxicity of radiation in pancreatic cancer cells.[36]
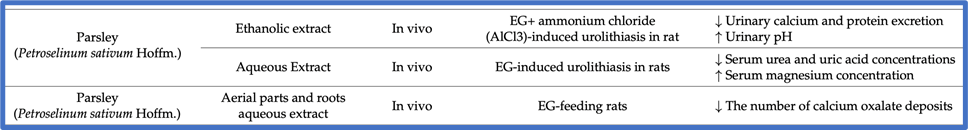
Phytoecdysteroids
Spinach is one of the few crop plants that produce large amounts of Phytoecdysteroids(PEs), of which 20-hydroxyecdysone is the significant component.
The content of 20-hydroxyecdysone in spinach leaves is about 0.01%, which is an order of magnitude lower than in medicinal plants.[37],[38]
Phytoecdysteroids in spinach support its defense system. PEs are potent anabolic compounds that support human health.
In 1982, the presence of plant anabolic compounds, known as ecdysteroids, were discovered in spinach.
Phytoecdysteroids like 20-hydroxyecdysone (“ecdysterone”) can exert a mild, non-hormonal anabolic/adaptogenic activity.[39]
A Source of Strength
Spinach has traditionally been considered a food that gives strength. Cue Popeye. His source of muscle growth and power? Spinach.

So, should you be afraid to eat spinach? Are the oxalates in spinach something to eschew? I don’t think so. I hope the science I’ve shared has helped convince you that spinach is a superfood, chock full of vitamins, minerals, and phytonutrients.
But what about the oxalates in spinach?
Although oxalates are considered bad anti-nutritive or even toxic, there are an overwhelming number of naturally occurring so-called toxins in the foods we eat daily. Our bodies can use these compounds to elicit benefits that are now beginning to be understood.
Avoiding the oxalates in spinach will only compromise gut immunity and digestive strength. Steering clear of green leafy vegetables and foods high in oxalates may cause other health issues. That’s why I believe that moderation and balance are key.
References
[1] Heller A, Witt-Geiges T. Oxalic acid has an additional, detoxifying function in Sclerotinia sclerotiorum pathogenesis. PLoS One. 2013 Aug 12;8(8):e72292. doi: 10.1371/journal.pone.0072292. PMID: 23951305; PMCID: PMC3741138.
[2] Fabio Palmieri, Aislinn Estoppey, Geoffrey L. House, Andrea Lohberger, SaskiaBindschedler, Patrick S.G. Chain, Pilar Junier, Chapter Two – Oxalic acid, a molecule at the crossroads of bacterial-fungal interactions, Editor(s): Geoffrey Michael Gadd, Sima Sariaslani, Advances in Applied Microbiology, Academic Press,Volume 106, 2019, Pages 49-77, ISSN 0065-2164, ISBN 9780128169759, https://doi.org/10.1016/bs.aambs.2018.10.001.
[3] Urbanek, Karen, HHP, Course-Creator, https://www.medicalnewstoday.com/articles/oxalic-acid
[4] Kim, HN., Kim, J.H., Chang, Y. et al. Gut microbiota and the prevalence and incidence of renal stones. Sci Rep 12, 3732 (2022). https://doi.org/10.1038/s41598-022-07796-y
[5] Siener, R. et al. The role of Oxalobacter formigenes colonization in calcium oxalate
stone disease. Kidney Int. 83, 1144–1149.
[6] Frassetto L, Kohlstadt I. Treatment and prevention of kidney stones: an update. Am Fam Physician. 2011 Dec 1;84(11):1234-42.
[7] Stepanova, N., Akulenko, I., Serhiichuk, T. et al. Synbiotic supplementation and oxalate homeostasis in rats: focus on microbiota oxalate-degrading activity. Urolithiasis (2022). https://doi.org/10.1007/s00240-022-01312-7
[8] Taylor E.N., Curhan G.C. Oxalate Intake and the Risk for Nephrolithiasis. J. Am. Soc. Nephrol. 2007;18:2198–2204. doi: 10.1681/ASN.2007020219
[9] Dai JC, Pearle MS. Diet and Stone Disease in 2022. J Clin Med. 2022 Aug 13;11(16):4740. doi: 10.3390/jcm11164740. PMID: 36012979; PMCID: PMC9410446.
[10] Ferraro P.M., Taylor E.N., Gambaro G., Curhan G.C. Soda and Other Beverages and the Risk of Kidney Stones. Clin. J. Am. Soc. Nephrol. 2013;8:1389–1395. doi: 10.2215/CJN.11661112.
[11] Johnson RJ, Perez-Pozo SE, Lillo JL, Grases F, Schold JD, Kuwabara M, Sato Y, Hernando AA, Garcia G, Jensen T, Rivard C, Sanchez-Lozada LG, Roncal C, Lanaspa MA. Fructose increases risk for kidney stones: potential role in metabolic syndrome and heat stress. BMC Nephrol. 2018 Nov 8;19(1):315. doi: 10.1186/s12882-018-1105-0. PMID: 30409184; PMCID: PMC6225702.
[12] Penniston K.L., Nakada S.Y., Holmes R., Assimos D.G. Quantitative Assessment of Citric Acid in Lemon Juice, Lime Juice, and Commercially-Available Fruit Juice Products. J. Endourol. 2008;22:567–570. doi: 10.1089/end.2007.0304.
[13] Zuckerman J.M., Assimos D.G. Hypocitraturia: Pathophysiology and medical management. Rev. Urol. 2009;11:134–144.
[14] Prezioso D, Strazzullo P, Lotti T, Bianchi G, Borghi L, Caione P, Carini M, Caudarella R, Ferraro M, Gambaro G, Gelosa M, Guttilla A, Illiano E, Martino M, Meschi T, Messa P, Miano R, Napodano G, Nouvenne A, Rendina D, Rocco F, Rosa M, Sanseverino R, Salerno A, Spatafora S, Tasca A, Ticinesi A, Travaglini F, Trinchieri A, Vespasiani G, Zattoni F; CLU Working Group. Dietary treatment of urinary risk factors for renal stone formation. A review of CLU Working Group. Arch Ital Urol Androl. 2015 Jul 7;87(2):105-20. doi: 10.4081/aiua.2015.2.105. Erratum in: Arch Ital Urol Androl. 2016 Mar;88(1):76. Ferraro, Manuel [added]. PMID: 26150027.
[15] Al-Yousofy, F.; Gumaih, H.; Ibrahim, H.; Alasbahy, A. Parsley! Mechanism as antiurolithiasis remedy. Am. J. Clin. Exp. Urol. 2017, 5, 55.
[16] Jafar, S.; Mehri, L.; Hadi, B. The antiurolithiasic activity of aqueous extract of Petroselinum sativum on ethylene glycolinduced kidney calculi in rats. In Proceedings of the International Conference on Chemical, Environmental and Biological Sciences, Pattaya, Thailand, 7–8 October 2011; pp. 1577–1583.
[17] Saeidi, J.; et. al. Therapeutic effects of aqueous extracts of Petroselinum sativum on ethylene glycol-induced kidney calculi in rats. Urol. J. 2012, 9, 361–366.
[18] Taylor EN, Fung TT, Curhan GC. DASH-style diet associates with reduced risk for kidney stones. J Am Soc Nephrol. 2009;20:2253–2259.
[19] Taylor EN, Stampfer MJ, Mount DB, Curhan GC. DASH-style diet and 24-hour urine composition. Clin J Am Soc Nephrol. 2010;5:2315–2322.
[20] Taylor EN, Curhan GC. Diet and fluid prescription in stone disease. Kidney Int. 2006;70:835–839
[21] Noonan SC, Savage GP. Oxalate content of foods and its effect on humans. Asia Pac J Clin Nutr. 1999 Mar;8(1):64-74. PMID: 24393738.
[22] Dai JC, Pearle MS. Diet and Stone Disease in 2022. J Clin Med. 2022 Aug 13;11(16):4740. doi: 10.3390/jcm11164740. PMID: 36012979; PMCID: PMC9410446.
[23] Velazquez E.G., Carrera S.P.P., Gutierrez R.M.P. Spinacia oleracea Linn Considered as One of the Most Perfect Foods: A Pharmacological and Phytochemical Review. Mini-Rev. Med. Chem. 2019;19:1666–1680. doi: 10.2174/1389557519666190603090347.
[24] Cartford M.C., Gemma C., Bickford P. Eighteen-Month-Old Fischer 344 Rats Fed a Spinach-Enriched Diet Show Improved Delay Classical Eyeblink Conditioning and Reduced Expression of Tumor Necrosis Factor α (TNFα) and TNFβ in the Cerebellum. J. Neurosci. 2002;22:5813–5816. doi: 10.1523/JNEUROSCI.22-14-05813.2002.
[25] Pezeshki-Nia S., Asle-Rousta M., Mahmazi S. Spinacia oleracea L. extract attenuates hippocampal expression of TNF-α and IL-1β in rats exposed to chronic restraint stress. Med. J. Islam. Repub. Iran. 2020;34:68–73. doi: 10.47176/mjiri.34.10.
[26] Elvira-Torales LI, Navarro-González I, Rodrigo-García J, Seva J, García-Alonso J, Periago-Castón MJ. Consumption of Spinach and Tomato Modifies Lipid Metabolism, Reducing Hepatic Steatosis in Rats. Antioxidants (Basel). 2020 Oct 24;9(11):1041. doi: 10.3390/antiox9111041. PMID: 33114278; PMCID: PMC7690917.
[27] Gutierrez R.M.P., Velazquez E.G. Glucopyranoside flavonoids isolated from leaves of Spinacia oleracea (spinach) inhibit the formation of advanced glycation end products (AGEs) and aldose reductase activity (RLAR) Biomed. Pharmacother. 2020;128:110299. doi: 10.1016/j.biopha.2020.110299.
[28] Panda V., Shinde P. Appetite suppressing effect of Spinacia oleracea in rats: Involvement of the short term satiety signal cholecystokinin. Appetite. 2017;113:224–230. doi: 10.1016/j.appet.2017.02.030.
[29] Choudhary D., Kothari P., Tripathi A.K., Singh S., Adhikary S., Ahmad N., Kumar S., Dev K., Mishra V.K., Shukla S., et al. Spinacia oleracea extract attenuates disease progression and sub-chondral bone changes in monosodium iodoacetate-induced osteoarthritis in rats. BMC Complement. Altern. Med. 2018;18:69. doi: 10.1186/s12906-018-2117-9
[30] Amirinejad A., Hekmatdoost A., Ebrahimi A., Ranjbaran F., Shidfar F. The effects of hydroalcoholic extract of spinach on prevention and treatment of some metabolic and histologic features in a rat model of nonalcoholic fatty liver disease. J. Sci. Food Agric. 2020;100:1787–1796. doi: 10.1002/jsfa.10215.
[31] Roberts J.L., Moreau R. Functional properties of spinach (Spinacia oleracea L.) phytochemicals and bioactives. Food Funct. 2016;7:3337–3353. doi: 10.1039/C6FO00051G.https://pubmed.ncbi.nlm.nih.gov/27353735/
[32] Lomnitski L., Bergman M., Nyska A., Ben-Shaul V., Grossman S. Composition, Efficacy, and Safety of Spinach Extracts. Nutr. Cancer. 2003;46:222–231. doi: 10.1207/S15327914NC4602_16.https://pubmed.ncbi.nlm.nih.gov/27353735/
[33] Panda V, Mistry K, Sudhamani S, Nandave M, Ojha SK. Amelioration of Abnormalities Associated with the Metabolic Syndrome by Spinacia oleracea (Spinach) Consumption and Aerobic Exercise in Rats. Oxid Med Cell Longev. 2017;2017:2359389. doi:10.1155/2017/2359389
[34] Maeda N, Kokai Y, Hada T, Yoshida H, Mizushina Y. Oral administration of monogalactosyl diacylglycerol from spinach inhibits colon tumor growth in mice. Exp Ther Med. 2013 Jan;5(1):17-22. doi: 10.3892/etm.2012.792. Epub 2012 Nov 1. PMID: 23251235; PMCID: PMC3524182.
[35] Chen YS, Li J, Neja S, Kapoor S, Tovar Perez JE, Tripathi C, Menon R, Jayaraman A, Lee K, Dashwood WM, Wang S, Zhang K, Kobayashi K, Rajendran P, Dashwood R. Metabolomics of Acute vs. Chronic Spinach Intake in an Apc-Mutant Genetic Background: Linoleate and Butanoate Metabolites Targeting HDAC Activity and IFN-γ Signaling. Cells. 2022 Feb 7;11(3):573. doi: 10.3390/cells11030573. PMID: 35159382; PMCID: PMC8834217.
[36] Akasaka H, Mizushina Y, Yoshida K, Ejima Y, Mukumoto N, Wang T, Inubushi S, Nakayama M, Wakahara Y, Sasaki R. MGDG extracted from spinach enhances the cytotoxicity of radiation in pancreatic cancer cells. Radiat Oncol. 2016 Nov 22;11(1):153. doi: 10.1186/s13014-016-0729-0. PMID: 27876069; PMCID: PMC5120455
[37] Fiorito S., Preziuso F., Epifano F., Scotti L., Bucciarelli T., Taddeo V.A., Genovese S. Novel biologically active principles from spinach, goji and quinoa. Food Chem. 2019;276:262–265. doi: 10.1016/j.foodchem.2018.10.018.
[38] Plant Physiology and Biochemistry 46 (2008) 844e854, Arch Insect Biochem Physiol. 2009 Dec;72(4):210-9, hypothesis, J. Chem. Ecol. 26 (2000) 2883e2896
[39] Hunyadi A, Herke I, Lengyel K, et al. Ecdysteroid-containing food supplements from Cyanotis arachnoidea on the European market: evidence for spinach product counterfeiting. Sci Rep. 2016;6:37322. Published 2016 Dec 8. doi:10.1038/srep37322