Given the ongoing discord within the scientific community regarding the short-term and long-term efficacy and safety of the different types of anti-SARS-CoV-2 vaccines, their experimental nature, and the availability of other therapeutic approaches,[1] such information should be universal and should be provided to every potential vaccine recipient. The safety and tolerance of COVID-19 vaccines must be carefully considered and studied even when the benefits may outweigh the disadvantages.[2]

Current research indicates that body weight, blood type, vitamin D and zinc status, and additional markers such as selenium are markers for determining your immunity or resistance to COVID. If we are healthy and weigh the markers I just stated, (besides old age) what is our actual risk of a severe or life-threatening COVID infection? If we focus on improving our health through diet, lifestyle, and normalizing the levels of these important nutrients for our immune system health, we could prevent more illnesses.
I believe that people should be informed about additional methods that can reduce their risk of contracting COVID-19. This should be provided for those who choose to forgo the vaccine, as well as those who want the vaccine and are interested in additional ways that they can bolster their resistance. As the pandemic continues, it is clear that the vaccine alone is not a guarantee of full-proof protection against the COVID virus.
What if we created a Covid-19 health report card and based on a score, we could better assess our risk-to-benefit when it comes to vaccinations?
Health Biomarker Risk Assessment:
- Metabolic Health Assessment – Body Mass Index (BMI) (optimal range is between 18-25), HGB A1C (optimal range is <5.8), fasting insulin, leptin, c-peptide, lipid profile, C-reactive Protein etc.
- Vitamin D levels – both 25 OH (optimal range is >40) and 125 diOH
- Zinc levels (optimal range is 80-130)
- Neutrophil-to-lymphocyte ratio (optimal range is <3:1 ratio) – a drop in lymphocytes and an increase in neutrophils is associated with worsening of COVID-19 and mortality.[3]
- Fibrinogen (Best if <375) and D-dimer (optimal range is <.4)
- Selenium (optimal range is 100-150)
- Blood type – blood group A might have a role in increased susceptibility to the COVID-19 infection, the blood group O might be somewhat protective.[4]
I would also include a history of chronic diseases (and severity), medications, and certain life-style risks such as smoking.
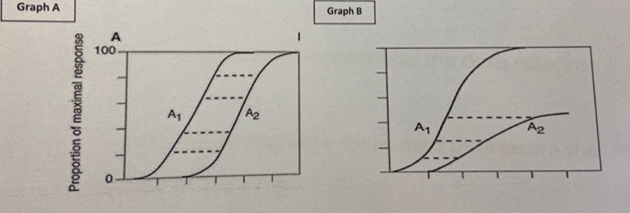
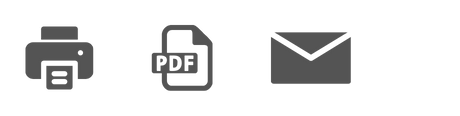
Interpreting the Data on Vaccine Efficacy
There are many lessons to learn from the way studies are conducted and results are presented. When including only relative risk reduction (RRR) while omitting absolute risk reduction (ARR), reporting bias is introduced, which affects the interpretation of vaccine efficacy.
“Vaccine efficacy is generally reported as a relative risk. It uses the relative risk (RR)—i.e., the ratio of attack rates with and without a vaccine—which is expressed as 1–RR. Ranking by reported efficacy gives relative risk reductions of 95% for the Pfizer–BioNTech, 94% for the Moderna–NIH, 91% for the Gamaleya, 67% for the Johnson and Johnson, and 67% for the AstraZeneca–Oxford vaccines. However, RRR should be seen against the background risk of being infected and becoming ill with COVID-19, which varies between populations and over time. Although the RRR considers only participants who could benefit from the vaccine, the ARR, which is the difference between attack rates with and without a vaccine, considers the whole population. ARRs tend to be ignored because they give a much less impressive effect size than RRRs: 1·3% for the AstraZeneca–Oxford, 1·2% for the Moderna–NIH, 1·2% for the J&J, 0·93% for the Gamaleya, and 0·84% for the Pfizer–BioNTech vaccines.”[5]
Unfortunately, comparing vaccines on the basis of currently available trial (interim) data is made even more difficult by disparate study protocols, including primary endpoints such as:
- What is considered a COVID-19 case, and when is this assessed?
- What are the types of placebo, study populations, background risks of COVID-19 during the study, duration of exposure, and different definitions of populations for analyses both within and between studies?
- What definitions of endpoints and statistical methods for efficacy were used?
- What are the serum levels of vitamin D, zinc, and selenium in the trial participants?
- What was the Body Mass Index?—we know that obese patients pose the highest risk.[6]
According to a recent systematic review and meta-analysis of 42 studies and 423,117 patients, chronic comorbidities, complications, and demographic variables including acute kidney injury, COPD, diabetes, hypertension, CVD, cancer, increased D-dimer, male gender, older age, current smoker, and obesity are clinical risk factors for a fatal outcome associated with COVID-19.[7] What about the rest of us?
We are left with the unanswered question as to whether a vaccine with a given efficacy in the study population will have the same efficacy in another population with different levels of COVID-19 background risks. This question is not trivial, because transmission intensity varies between countries and is affected by factors, such as public health interventions and virus variants.[8]
Concerns about the mRNA Vaccines
The current COVID-19 vaccines use different types of technology, with some being introduced for the first time, and some that have been rushed into testing, bypassing animal experimentation. Recent research into the physiological effects of these agents reveal that they might slowly induce stimulation of myeloid or plasmacytoid dendritic cells, generating an imbalance in the downstream cytokine pathways that play a crucial role in autoimmunity and autoinflammation.[9]
The mRNA vaccines may actually bind to pattern recognition receptors in endosomes or cytosol, which can in turn activate several pro-inflammatory cascades, including the assembly of inflammasome platforms, the type I interferon (IFN) response and the nuclear translocation of the transcription factor nuclear factor (NF)-kB.[10] Pathogens may trigger autoimmunity if a part of these epitopes resemble those of similar structures expressed on human cells, as demonstrated in several post-infectious diseases that trigger many of the well-known autoimmune diseases. This process is likely in the context of genetic predisposition, such as in those with the HLA-DQB1 gene,[11] which is strongly suspected to be the cause of the narcolepsy that occurred in hundreds of children after their vaccination against the novel influenza A (H1N1) virus (“swine flu”), a vaccine that was later discontinued.
This process is known as molecular mimicry. Kanduc and Shoenfeld recently reported frequent similarities between numerous short sequences from the SARS-CoV-2 spike protein, which the virus uses to enter the cell, and human proteins.[12] The present mRNA vaccines are designed to stimulate a human cell to become a pathogen-manufacturing site in which the cell produces the spike protein, which ultimately triggers the immune system to produce neutralizing antibodies against the spike protein and which may cross-react with one of the self-antigens and trigger an autoimmune disease,[13] as recently reported with the AstraZeneca and Johnson & Johnson vaccines. Vaccine-associated autoimmunity is a well-known phenomenon attributed to either the cross-reactivity between antigens and/or the effect of adjuvant.[14]
In addition to molecular mimicry, mRNA vaccines may give rise to a cascade of immunological events, eventually leading to the aberrant activation of the innate and acquired immune system.[15] Up-regulation of these immunological pathways is widely considered to be the basis of several immune-mediated diseases, especially in genetically predisposed individuals who have an impaired clearance of nucleic acids.[16] Another concern, in the case of a switch in the immune system and in people with genetic predisposition is the risk of the continuous production of the spike protein and corresponding antibodies, which could lead to a state of chronic inflammation.[17]
In these unprecedented times, it is essential to use the skills of critical thinking to arrive at a balanced perspective. According to the Children’s Hospital of Philadelphia,[18] the mRNA vaccines are not expected to have long-term negative effects for a few reasons:
- First, most negative effects occur within 6 weeks of receiving a vaccine, which is why the FDA asked the companies to provide 8 weeks of safety data after the last dose.
- Second, the mRNA in the vaccine breaks down quickly because our cells need a way to stop mRNA from making too many proteins or too much protein.
- Third, even if for some reason our cells did not break down the vaccine mRNA, the mRNA stops making the protein within about a week, regardless of the body’s immune response to the protein.
These observations and assertions add to the case that the mRNA vaccines may be safe, yet there is still much about the long-term effects that we don’t know.
Potential Risks Need to be Communicated
Reviewing this data reminds us that there are potential risks associated with the current COVID-19 vaccines. As I said at the beginning of this post, the risks should be communicated to those who are getting the vaccine, and there should be a consent form included so that each individual can make a personal decision weighing the risk-to-benefit ratio. We should also be evaluating the relative risk of severe illness and death from Covid-19 for those who are unvaccinated based on the previously mentioned biomarker health assessment and especially BMI, blood type, vitamin D and zinc levels in “less vulnerable” populations.

In general, I approach pharmaceuticals with caution and seek out natural alternatives to support my bodies innate healing capacity. This is based in my deeply rooted personal belief system. I am also well aware of the long list of drugs and chemicals that were approved by the FDA and subsequently taken off of the market when risks emerged. The reality is that almost every drug has long-term risks, even something as common as antibiotics. Many antibiotics, especially the fluoroquinolone class of antibiotics (such as Cipro), cause tendon weakness and ruptures. This was not known when the drugs were approved. Fluoroquinolones destroy collagen and connective tissue and cause DNA damage and mitochondrial disorder in tendon cells.[19] All antibiotics damage the gut microbiome and increase risk for secondary infections such as yeast infections, and they reduce the benefits of immunotherapy, which is an important treatment for many cancers (antibiotics cause dysbiosis or loss of microbial diversity and have been associated with a poor treatment response to immune checkpoint inhibitors).[20],[21] The cumulative intake of antibiotics is associated with significantly increased risk for several cancers, including breast[22],[23] and colon cancer.[24],[25] Even more recently, antibiotic administration was found to be associated with reduced efficacy of neoadjuvant therapy and poor prognosis in breast cancer patients. Despite the evidence, potential risks are rarely shared when prescribing an antibiotic.[26]
Given the valid concerns on well-recognized short-term and long-term safety issues—such as antibody-dependent enhancement (ADE) and other processes like molecular mimicry and potential genomic transformation, the experimental nature of the vaccination process, and the limited short-term follow-up in the main trials—obtaining informed consent that discloses the risks before deciding on any vaccine is reasonable and appropriate.
Myocarditis Risk with the COVID-19 Vaccine in Adolescents
Researchers that relied heavily on the Vaccine Adverse Event Reporting System (VAERS) data to characterize myocarditis risk with the COVID-19 vaccine in adolescents, particularly young boys, revealed in a new report by Tracy Høeg, MD, PhD, of the University of California Davis and colleagues, that rates of “cardiac adverse events” after the second vaccine dose were higher than previous CDC estimates. This was 162 per million among boys ages 12 to 15 and 94 per million among boys ages 16 to 17. (Rates were much lower for girls, at about 13 per million for each age group.)
The authors also concluded that the risk of hospitalization for cardiac adverse events following vaccination is higher than the risk of being hospitalized with COVID for healthy boys in both age groups.[27]
Antibody Protection and Booster Shots
A decline in antibody levels against Covid-19 among some people who got vaccinated late last year is being cited as part of the scientific case for why millions of Americans need booster shots. But in reality, that basis is theoretical and not based on concrete evidence. There is considerable uncertainty about what detectable antibodies really mean when it comes to protection. And a lack of standardization among the commercially available tests for antibodies makes it even harder to decipher the results.[28]
Antibody tests only give one view into the body’s collection of defenses against the coronavirus. In fact, it’s just a subset of antibodies, made in response to the virus or a shot of the vaccine, that neutralize the spike protein on the virus. The spike protein is what enables the coronavirus to break into cells and replicate. “We have a mix of antibodies. Some of them are very good and protective. Some are not as protective,” and each person will have their own mix of these different types of antibodies, says Ali Ellebedy, an immunologist at Washington University School of Medicine in St. Louis who’s studying the antibody response to the coronavirus.[29]
Don’t forget the immune system is more than just antibodies, so even with low detectable levels in your blood, you’re not defenseless. “Antibody tests — it’s really probing just one part of your immune system,” says Elitza Theel, who directs the Infectious Diseases Serology Laboratory at the Mayo Clinic.
Your immune system really kicks into action if your body encounters the coronavirus. At that point, it generates new antibodies to block the virus and taps another line of defense — called T cells — which clear out the infected cells that have been converted into factories where the virus can multiply.[30]
As we deal with the delta variant, we may soon have to take on the apparent vaccine resistant lambda variant.[31] In addition, the WHO is now monitoring yet another new coronavirus variant called “mu,” which it says could potentially also evade immunity provided by a vaccine or previous coronavirus infection.[32]
Unfortunately, the current pandemic isn’t close to being over. Therefore, there has never been a more critical and urgent time to optimize our health and immune systems, which could be our strongest weapon against illness. As I said before, it is essential to use the skills of critical thinking to arrive at a balanced perspective. The mRNA vaccines are not expected to have long-term negative effects, but people should be aware of them before getting one. Each person, depending on their vulnerability health-wise, lifestyle habits and levels of exposure, needs to weigh the pros and cons of a vaccine and make educated decisions before getting one. Information by the Physicians for Informed Consent comparing the efficacy and risk of COVID-19 vaccines versus the risk of COVID-19 can be obtained at https://physiciansforinformedconsent.org/COVID-19-vaccines/
References
[1] Dagan N, Barda N, Kepten E, et al. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. N Engl J Med. 2021;384(15):1412-1423. doi:10.1056/NEJMoa2101765
[2] Novak N, Tordesillas L, Cabanillas B. Adverse rare events to vaccines for COVID-19: From hypersensitivity reactions to thrombosis and thrombocytopenia [published online ahead of print, 2021 Jul 12]. Int Rev Immunol. 2021;1-10. doi:10.1080/08830185.2021.1939696
[3] Liu Y. Du X, Chen J et al. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19, Journal of Infection (2020) 81(1) e6-e12, DOI: 10.1016/j.jinf.2020.04.002
[4] Göker H, Aladağ Karakulak E, Demiroğlu H, Ayaz Ceylan ÇM, Büyükaşik Y, Inkaya AÇ, Aksu S, Sayinalp N, Haznedaroğlu IC, Uzun Ö, Akova M, Özcebe OI, Ünal S. The effects of blood group types on the risk of COVID-19 infection and its clinical outcome. Turk J Med Sci. 2020 Jun 23;50(4):679-683. doi: 10.3906/sag-2005-395. PMID: 32496734; PMCID: PMC7379446.
[5] Brown RB. Outcome reporting bias in COVID-19 mRNA vaccine clinical trials. Medicina (Kaunas) 2021;57:199.
[6] Mason KE, Maudsley G, McHale P, Pennington A, Day J, Barr B. Age-Adjusted Associations Between Comorbidity and Outcomes of COVID-19: A Review of the Evidence From the Early Stages of the Pandemic. Front Public Health. 2021 Aug 6;9:584182. doi: 10.3389/fpubh.2021.584182. PMID: 34422736; PMCID: PMC8377370.
[7] Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect Dis. 2021 Aug 21;21(1):855. doi: 10.1186/s12879-021-06536-3. PMID: 34418980.
[8] Olliaro P, Torreele E, Vaillant M. COVID-19 vaccine efficacy and effectiveness-the elephant (not) in the room. Lancet Microbe. 2021;2(7):e279-e280. doi:10.1016/S2666-5247(21)00069-0
[9] Talotta R. Do COVID-19 RNA-based vaccines put at risk of immune-mediated diseases? In reply to “potential antigenic cross-reactivity between SARS-CoV-2 and human tissue with a possible link to an increase in autoimmune diseases”. Clin Immunol. 2021;224:108665. doi:10.1016/j.clim.2021.108665
[10] Reikine S., Nguyen J.B., Modis Y. Pattern Recognition and Signaling Mechanisms of RIG-I and MDA5. Front. Immunol. 2014;5 doi: 10.3389/fimmu.2014.00342. 342-undefined
[11] Khamsi R. Rogue antibodies could be driving severe COVID-19. Nature. 2021;590(7844):29-31. doi:10.1038/d41586-021-00149-1
[12] Kanduc D, Shoenfeld Y. Molecular mimicry between SARS-CoV-2 spike glycoprotein and mammalian proteomes: implications for the vaccine. Immunol Res. 2020;68(5):310-313. doi:10.1007/s12026-020-09152-6
[13] Vojdani A, Kharrazian D. Potential antigenic cross-reactivity between SARS-CoV-2 and human tissue with a possible link to an increase in autoimmune diseases. Clin Immunol. 2020;217:108480. doi:10.1016/j.clim.2020.108480
[14] Talotta R. Do COVID-19 RNA-based vaccines put at risk of immune-mediated diseases? In reply to “potential antigenic cross-reactivity between SARS-CoV-2 and human tissue with a possible link to an increase in autoimmune diseases”. Clin Immunol. 2021;224:108665. doi:10.1016/j.clim.2021.108665
[15] Vojdani A, Kharrazian D. Potential antigenic cross-reactivity between SARS-CoV-2 and human tissue with a possible link to an increase in autoimmune diseases. Clin Immunol. 2020;217:108480. doi:10.1016/j.clim.2020.108480
[16] Pelka K, Shibata T, Miyake K, Latz E. Nucleic acid-sensing TLRs and autoimmunity: novel insights from structural and cell biology. Immunol Rev. 2016;269(1):60-75. doi:10.1111/imr.12375
[17] Mazraani M, Barbari A. Anti-Coronavirus Disease 2019 Vaccines: Need for Informed Consent. Exp Clin Transplant. 2021 Aug;19(8):753-762. doi: 10.6002/ect.2021.0235. PMID: 34407747.
[18] Questions and Answers about COVID-19 Vaccines https://www.chop.edu/centers-programs/vaccine-education-center/making-vaccines/prevent-covid, July 21 2021
[19] Judith Sendzik, Mehdi Shakibaei, Monika Schäfer-Korting, Ralf Stahlmann, Fluoroquinolones cause changes in extracellular matrix, signalling proteins, metalloproteinases and caspase-3 in cultured human tendon cells,
Toxicology, Volume 212, Issue 1, 2005, Pages 24-36, ISSN 0300-483X, https://doi.org/10.1016/j.tox.2005.04.002.
[20] Naqash AR, Kihn-Alarcón AJ, Stavraka C, Kerrigan K, Maleki Vareki S, Pinato DJ, Puri S. The role of gut microbiome in modulating response to immune checkpoint inhibitor therapy in cancer. Ann Transl Med. 2021 Jun;9(12):1034. doi: 10.21037/atm-20-6427. PMID: 34277834; PMCID: PMC8267312
[21] Huang XZ, Gao P, Song YX, Xu Y, Sun JX, Chen XW, Zhao JH, Wang ZN., Antibiotic use and the efficacy of immune checkpoint inhibitors in cancer patients: a pooled analysis of 2740 cancer patients.
Oncoimmunology. 2019; 8(12):e1665973.
[22] Velicer CM, Heckbert SR, Lampe JW, Potter JD, Robertson CA, Taplin SH. Antibiotic use in relation to risk of
breast cancer. JAMA. 2004;291:827-835.
[23] Johanna Simin, Rulla M. Tamimi, Lars Engstrand, Steven Callens, Nele Brusselaers, Antibiotic use and the risk of breast cancer: A systematic review and dose-response meta-analysis, Pharmacological Research, Volume 160, 2020,105072, ISSN 1043-6618, https://doi.org/10.1016/j.phrs.2020.105072.
[24] Qu G, Sun C, Sharma M, Uy JP, Song EJ, Bhan C, Shu L. Is antibiotics use really associated with increased risk of colorectal cancer? An updated systematic review and meta-analysis of observational studies. Int J Colorectal Dis. 2020 Aug;35(8):1397-1412. doi: 10.1007/s00384-020-03658-z. Epub 2020 Jun 6. PMID: 32504337.
[25] Cao Y, Wu K, Mehta R, Drew DA, Song M, Lochhead P, Nguyen LH, Izard J, Fuchs CS, Garrett WS, Huttenhower C, Ogino S, Giovannucci EL, Chan AT. Long-term use of antibiotics and risk of colorectal adenoma. Gut. 2018 Apr;67(4):672-678. doi: 10.1136/gutjnl-2016-313413. Epub 2017 Apr 4. PMID: 28377387; PMCID: PMC5628103.
[26] Zhang X, Yu L, Shi J, Li S, Yang S, Gao W, Yang S, Cheng M, Wang H, Guo Z, Geng C. Antibiotics modulate neoadjuvant therapy efficiency in patients with breast cancer: a pilot analysis. Sci Rep. 2021 Jul 7;11(1):14024. doi: 10.1038/s41598-021-93428-w. PMID: 34234229; PMCID: PMC8263554.
[27] Tracy Beth Høeg MD, PhD1; Allison Krug, MPH2; Josh Stevenson3; John Mandrola,
MDSARS-CoV-2 mRNA Vaccination-Associated Myocarditis in Children
Ages 12-17: A Stratified National Database Analysis, medRxiv preprint doi: https://doi.org/10.1101/2021.08.30.21262866; this version posted September 8, 2021; Medscape article https://www.medpagetoday.com/special-reports/exclusives/94530?xid=nl_covidupdate_2021-09-16&eun=g1065123d0r&utm_source=Sailthru&, 09/16/2021
[28] https://publichealth.jhu.edu/2020/the-potential-and-limits-of-antibody-testing, The Potential—and Limits—of Antibody Testing retrieved 09/07/2021
[29] https://todayheadline.co/covid-antibody-tests-cant-measure-your-immunity-not-yet-shots-health-news-npr/, retrieved 09/08/2021
[30] https://www.npr.org/sections/health-shots/2021/08/28/1031287076/antibody-tests-should-not-be-your-go-to-for-checking-covid-immunity retrieved 02/08/2021
[31] Izumi Kimura, Yusuke Kosugi, Jiaqi Wu, Daichi Yamasoba, Erika P Butlertanaka, Yuri L Tanaka, Yafei Liu, Kotaro Shirakawa, Yasuhiro Kazuma, Ryosuke Nomura, Yoshihito Horisawa, Kenzo Tokunaga, Akifumi Takaori-Kondo, Hisashi Arase, The Genotype to Phenotype Japan (G2P-Japan) Consortium, Akatsuki Saito, So Nakagawa, Kei Sato, SARS-CoV-2 Lambda variant exhibits higher infectivity and immune resistance, bioRxiv 2021.07.28.454085; doi: https://doi.org/10.1101/2021.07.28.454085
[32] https://www.cnbc.com/2021/09/01/who-says-it-is-monitoring-a-new-covid-variant-called-mu.html, retrieved 9/02/2021