“I have no data yet. It is a capital mistake to theorize before one has data. Insensibly one begins to twist facts to suit theories instead of theories to suit facts.” ~Sherlock Holmes.
Conventional medicine has long been wary of traditional herbal medicine, particularly when it comes to the potential interactions of herbs and pharmaceutical drugs. However, the focus of conventional medicine always seems to be on the negative interactions of herbs and drugs, when in fact, herb-drug interactions can often be positive.
Examples of positive herb-drug interactions include:
- Herb-drug synergy, where the herb potentiates the effects of the drug, allowing for a lower dosage of the drug
- Ameliorating side-effects of the drug
- Protecting vital organs from short and long-term toxicity
- Inhibiting drug resistance
I have been in practice for nearly thirty years, intelligently and safely combining comprehensive herbal formulations with hundreds of different drugs for all kinds of conditions and diseases. Based on my clinical experience and my ongoing comprehensive and careful review of scientific literature, my opinion is that the extreme warnings and cautionary articles published by both the media and various medical institutions is for the most part based on unsubstantiated theories and misinformation about plants and their physiological effects.
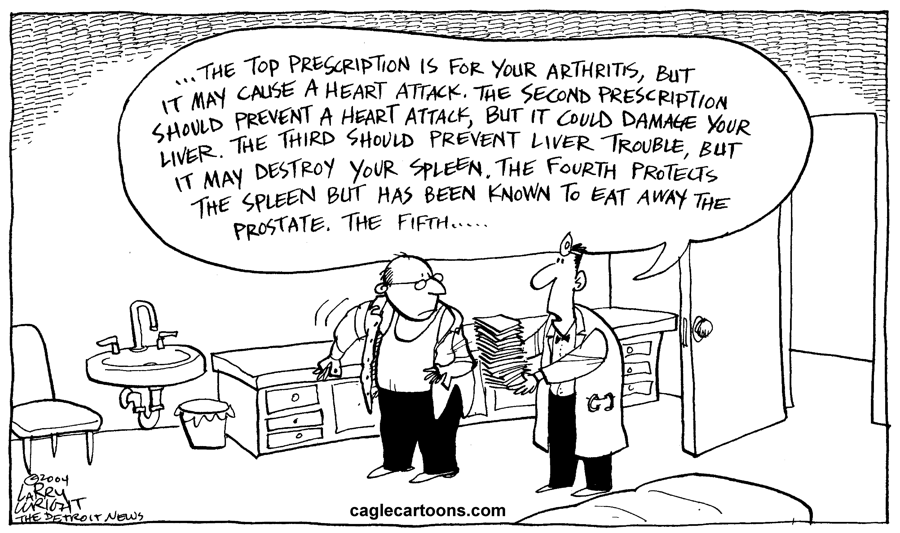
Certainly, we should proceed with caution and common sense, carefully reviewing scientific studies before we prescribe herbs and herbal formulas in tandem with drugs. There are definitely cases of proven herb-drug interactions. However, there are few people with significant experience—much less expertise—in this specialized area of medicine. Consequently, both the public and health professionals in search of guidance are often convinced that all herbs should be strictly avoided. This approach is based on unwarranted concerns deduced from negative reports and a lack of understanding about the physiological effects of plants. This is also the primary reason why doctors neglect to discuss this issue with their patients, the majority of whom are already taking herbal supplements. Meanwhile, many patients are taking multiple drugs simultaneously. The safety data on drug-drug interactions is severely lacking, and this, I believe, is a much greater risk.
A Case of Misplaced Worry
Something that I have always found incongruous is the exaggerated worry over herb-drug interactions, but the apparent lack of concern about drug-to-drug interactions. Here’s a common scenario: Most people have more than one doctor, often including several specialists. It’s not unusual for one doctor to precribe one or more drugs for a patient, with other doctors prescribing additional drugs for other conditions, or to treat the side effects of the drugs. There is little to no research on the effects of patients taking a multitude of drugs. Bear in mind that in general, herbs are much safer than drugs and do not function like drugs. That being said, it is important that patients be under the care of an expert in natural medicine and should not self-prescribe or take supplements that are not professional-grade and verified for quality, purity and potency.
Another concern about pharmaceutical drugs is their effect on the environment. With so many people taking and excreting drugs, drinking water in many places is now contaminated with low levels of pharmaceuticals. In an investigation by the Associated Press, drinking water supplies in 24 major metropolitan areas were found to include drugs—including antibiotics, hormones, mood stabilizers, and other drugs.1
How Misinformation about Herbs Affects Patient Treatment
Conventional doctors often recommend that patients avoid herbs, particularly if they are undergoing treatment for cancer. This is highly unfortunate, because herbs have a great deal to offer in a comprehensive plan for maintaining health and effectively managing cancer. Doctors routinely advise patients to avoid herbs prior to surgery because they are ‘blood thinners’—assuming that the herbs act like coumadin or aspirin. In reality, many herbs, such as yarrow (Achillea millefolium), are blood moving, discourage ‘abnormal’ blood clots/thrombosis, yet are able to improve blood coagulation when needed, such as wound healing. This is just one example of the many erroneous theories that are accepted with no concrete data to back them up.
The focus of my practice is to help improve health, which encompasses much more than simply the eradication of illness. With this goal in mind, and using the assessment tools of the Eclectic Triphasic Medical System (ETMS), I provide protocols that routinely incorporate several herbal formulas, often in tandem with drugs. In three decades of practice, I have found that integrating an herbal protocol into a treatment plan does not diminish the efficacy of drugs, nor does it increase toxicity. Instead, the results show that the herbal protocol improves effectiveness, which often means patients are able to take a lower dosage of pharmaceutical drugs.
Three Important Distinct Factors to Evaluate in Reviewing HDIs
- Pharmacokinetics (PKs): Before considering HDIs, it is essential to consider the following processes in relation to the drug: 1) liberation, 2) absorption, 3) distribution, 4) metabolism and 5) excretion. Ideally, the concentration of drug should be measured at the site of action of the drug (at the receptor or tissue), rather than plasma or serum levels. Within HDI studies, what is defined as an interaction is based on specific drugs metabolizing enzymes responsible for excretion, and the impact of an herb (or a specific herb compound) and how the compound might affect the related enzyme by either inducing it or suppressing it. In general, it is only this factor that is considered when evaluating HDIs. Unfortunately, even this is not carefully studied, because whole herbs, herbal extracts, and herbal formulations differ from herb isolates. In addition, the dosage needed to significantly affect induction or suppression is not adequately studied. Other considerations include types of foods eaten, amount of stress, activity, and sleep. This is one reason why you can not depend on PKs as the sole means to evaluate HDIs.
Evaluating drug-drug, nutrient-drug, or botanical-drug interactions based on the cytochrome P450 enzyme pathway for metabolism is difficult. It’s important to note that 50% of all drugs marketed today use the cytochrome P450 enzyme pathway for metabolism and thus may cause drug-drug, nutrient-drug, or botanical-drug interactions.
In brief, the cytochrome P4503A (CYP3A) subfamily is largely found in hepatocytes, with some presence in the intestine. Together with the transport protein P-glycoprotein (PGP) present in the small intestine, these two systems regulate the metabolism of drugs and nutrients. Many foods, food components, and botanical supplements interact with the CYP3A and PGP metabolism, but even more importantly, genotypic variability plays a significant role in how well one metabolizes and detoxifies various drugs. The effects of herbs on CYP3A and PGP is dose sensitive, suggesting that high doses of herbs are required to modulate CYP and PGP activities.
One problem in discovering the truth about potential HDI’s is that much of the published research is either in vitro, perfomed on animal models, done with isolates (not whole herbs), and/or based on high dosages of these compounds. As a result, there are many theoretical herb-drug interactions that have never been observed clinically. An additional issue is that basing interaction data solely on P450 3A and PGP may not provide the most accurate model of HDI’s. The pertinent clinical question is, “Does a particular herb either cause a select drug to be less effective or increase its toxicity?” Until high quality human data is available, extrapolations made from in vitro models using supra-physiological concentrations of isolated constituents, and animal models using unrealistic dosing, may lead to misleading understandings of the potential of HDI’s.
- Pharmacogenomics: This is the study of how genes affect a person’s response to drugs. This relatively new field combines pharmacology (the science of drugs) and genomics (the study of genes and their functions) to develop effective, safe medications and doses that can be tailored to a person’s genetic makeup. I believe pharmacogenomics is even more important than PKs yet this is very seldom applied when dosing drugs.
- Pharmacodynamics (PDs): This explains the relationship between the dose and response—what actually occurs when you mix a specific drug with a specific herb. A drug’s pharmacodynamics can be affected by physiologic changes due to disorders, aging, or other drugs. Disorders that affect pharmacodynamic responses include genetic mutations, malnutrition, Parkinson’s disease, insulin resistance, and diabetes mellitus. Pharmacodynamics is most relative when it comes to studying HDIs and is not theoretical, but reflects the actual net-effect when an herb and drug are taken concurrently.
The Positive Effects of Herb-Drug Interactions
Botanicals naturally have a multi-faceted nature, which makes them eminently suitable for addressing the wide range of issues associated with complex diseases such as cancer. In my practice, I’ve observed that the synergestic actions of herbs can even help to buffer the effects of conventional chemotherapeutic drugs.
Current research supports my long-held observation that the marriage of herbs and conventional drugs can be successful and beneficial. A recent evaluation of herb-drug interactions and research published in The Journal of Alternative and Complementary Medicine revealed a positive outcome that will hopefully help to shift awareness within the medical profession. In their evaluation of 17 studies conducted worldwide on HDI-induced pharmacodynamic interactions, the researchers concluded that:
- The concomitant use of herbal and conventional drugs accelerates the possibility of clinically significant herb-drug interactions (HDIs).
- The researchers evaluation found a generally positive view of effects, which involved synergism between the herbs and drugs and reduced toxicity.2
The Role of Herbal Medicine in Cancer Therapies
Herbal medicine has been the foundation of treatment for human maladies since ancient times, and continues to be an essential part of culturally based healing traditions in many cultures worldwide. As our respect for botanical medicine has grown, numerous herbs, including those traditionally used in Chinese medicine, are being incorporated as remedies for disease management and treatment in Western countries.3
Consider the following:
- 69% of anticancer drugs approved between the 1980s and 2002 are either natural products or have been developed based on knowledge gained from natural products.4
- About three quarters of plant-derived drugs in clinical use today came to the attention of pharmaceutical companies because of their use in traditional medicines.5
Because botanicals contain a variety of organic chemical complexes, they usually act on multiple targets. I consider this to be a significant benefit—for example, a potential advantage of phytochemicals is that they may act through multiple pathways and thus, reduce the development of resistance by cancer cells.6
The following summarizes compelling pre-clinical data regarding herb/drug interactions from scientific research papers:
- Anti-cancer efficacy in vitro and in vivo (but without evidence of toxicity) against multiple tumor types;
- Broad therapeutic window and no expected dose-limiting toxicity;
- Synergistic anti-cancer activity with multiple approved cancer therapies including chemotherapy and radiation therapy;
- Potential for ubiquitous use (for all stages of cancer) including adjuvant to surgery, radiation, chemotherapy, targeted agents and immune therapy; and maintenance for survivors to improve quality of life and lifespan.
Botanicals are the main “players” or core components in the ETMS approach to health, which takes into consideration the entire mileu of the individual within their environment. It is a more complex task for the physician to prescribe and monitor botanicals in tandem with drugs—no question about it. But being able to confidently assess the risk-to-benefit and safely incorporate botanicals allows for a more elegant, comprehensive, and ultimately successful approach to healing and medicine.
References
- http://www.webmd.com/a-to-z-guides/features/drugs-in-our-drinking-water?page=3, March 10, 2008
- Jin Gyu Choi, MS, Sang Min Eom, BS, Jaeyoung Kim, BS, et al. A Comprehensive Review of Recent Studies on Herb-Drug Interaction: A Focus on Pharmacodynamic Interaction. The Journal of Alternative and Complementary Medicine, Vol 22, No. 4, 2016, pp. 262-279.
- Wang CZ, Luo X, Zhang B, et al. Ginseng enhances anti-cancer effect of 5-fluorouracil on human colorectal cancer cells. Center for Herbal Medicine Research, The University of Chicago; Cancer Chemotherapy and Pharmacology Journal; 2006 Sep 29. Hsieh TC, Wu JM. Department of Biochemistry and Molecular Biology, New York Medical College, Valhalla; Published: International Journal of Oncology, 2006 Nov;29(5):1215-22.
- Newman DJ, Cragg GM. Natural products as sources of new drugs over the last 25 years. J Nat Prod 2007;70:46–77.
- Abelson PH. Medicine from Plants. Science 1990; 247:513.
- Sagar SM, Yance D, Wong RK. Natural health products that inhibit angiogenesis: a potential source for investigational new agents to treat cancer-Part 1.Curr Oncol. 2006 Jun;13(3):99-107.