Glyphosate, Not Gluten, Is the True Villain

‘There is nothing more deceptive than an obvious fact.’~Sherlock Holmes Over the past 30 years, gluten has become the number one villain among foods. At one time, an allergy to gluten was rarely seen. Today, almost 3 million people in the United States have celiac disease, a serious immune reaction to the protein in wheat, […]
Botanical Compounds in Cancer Combination Therapies

There is an extensive body of research demonstrating in vitro and in vivo (animal and human) synergy between natural products and anti-cancer drugs including chemotherapy, targeted agents, and immunotherapy against primary cancer, cancer resistance, and particularly cancer stem cells.
Are “Wonder Drugs” the Answer to Curing Cancer?

I often find myself thinking that modern medicine has it all wrong when it comes to treating cancer. Miraculous new treatments for cancer make headlines every day, but what are the long-term results of these treatments? Are these wonder drugs truly extending life, and more importantly, are they enhancing quality of life? According to a […]
Thriving in The Face of a Cancer Diagnosis

If you have recently been diagnosed with advanced cancer or another serious life-threatening disease, remember that everything you might think about it—positive or negative—is merely an interpretation. You are the one who decides how you will relate to the cancer diagnosis. “Success is never final, and failure is never fatal” -John Wooden My advice, based […]
Understanding Neutrophil to Lymphocyte Ratio (Part 2): Research Demonstrating its Role as a Valuable Prognostic Marker in Cancer
Understanding Neutrophil to Lymphocyte Ratio (Part 2): Research Demonstrating its Role as a Valuable Prognostic Marker in Cancer A large body of research (as well as my clinical observations) point to chronic inflammation as a powerful force in the initiation, growth, and spread of cancer. As a result, an essential component of my protocol for […]
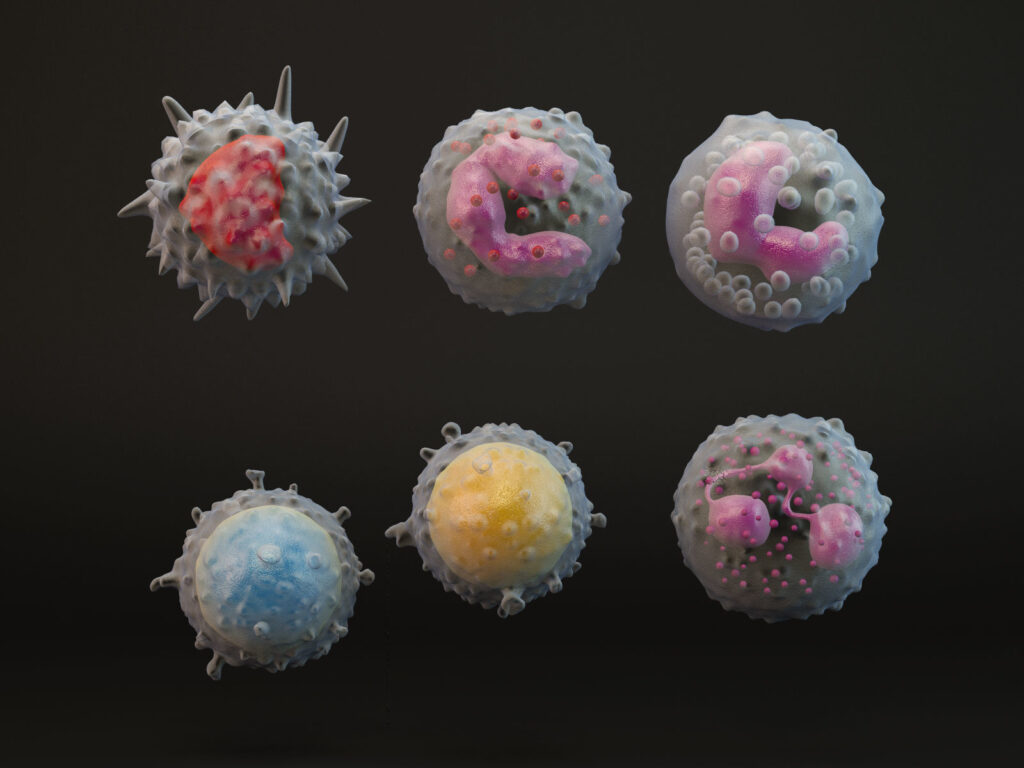
Understanding Neutrophil to Lymphocyte Ratio: The Most Important and Overlooked Biomarker of Systemic Inflammation in Cancer: Part 1

Inflammation is an essential part of our body’s immune defense. When we encounter pathogens such as bacteria, viruses, or parasites, our body responds with inflammation to fight the invaders and increase immune response. In these instances, inflammation is beneficial. But inflammation has a dark side—left unchecked, it can wreak havoc on cells, tissues, and organs. […]
‘Misrepresentation of ‘Integrative Oncology’ in the Literature: Clearing up Misperceptions and Recognizing the Validity of Herbal Medicine at the Forefront of ‘Unified Medicine’

I recently read a paper entitled “Integrative Oncology” 1 published in a peer-reviewed medical journal. To say I was shocked at the misrepresentation presented as “fact” is an understatement. I am strongly compelled to offer a rebuttal to this article. I can only hope that those who most need the perspective of someone who has […]
Enhancing Cellular Defense Mechanisms with Adaptogens

Enhancing Cellular Defense Mechanisms with Adaptogens Aging is associated with a decrease in adaptive abilities along with increased vulnerability to stress. At the same time, aging is a complex process involving a persistent activation of some stress response systems, often involving transcriptional reprogramming, and the activation of vitagenes, which can be consider a ‘geroprotective’ adaptation.13 […]
Pesca-Flexa-Vegetarianism – The Ideal Mediterranean-Style Diet for Optimal Health

I’m often asked what I consider to be the healthiest diet. Through decades of nutritional research and experimentation, I’m convinced that a diet of primarily organic, plant-based Mediterranean foods—including whole grains, fruits, vegetables, nuts, legumes, eggs, dairy products (cow, goat and sheep milk derived) and healthy fats (mostly olive oil), with fish and seafood playing […]
