The Healthiest Fish to Eat for Heart and Brain Health
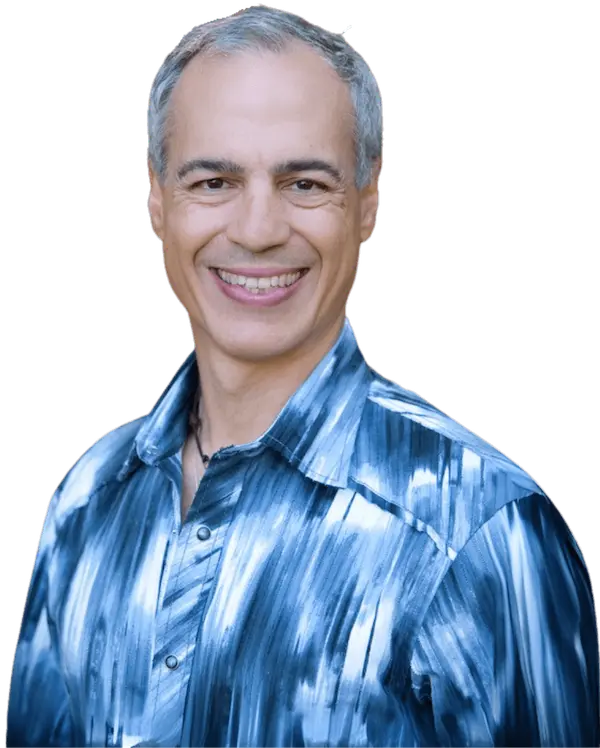
By Donnie Yance As a Clinical Master Herbalist and Certified Nutritionist who has studied the Mediterranean diet for over four decades, I recommend incorporating fish as a cornerstone of a heart- and brain-healthy dietary pattern. Based on extensive research and traditional dietary wisdom, here are my top recommendations: The Symphony