By Donnie Yance
“Conformity is the jailer of freedom and the enemy of growth.” – John F. Kennedy, 35th U.S. president
It’s the new year again and weight loss goals are on the minds of millions of people in America and around the world.
Before you dive into this blog you may want to review several of my previous blogs including (August 3, 2023), “Are Diabetic Weight Loss Drugs Really The New Diet? Discover the Benefits Of Intuitive Eating.”
GLP−1 Receptor Agonists For the Treatment of Obesity
Glucagon-like peptide-1 receptor (GLP-1R) agonists represent a groundbreaking class of medications that target incretin hormone pathways. Incretins stimulate the pancreas to release insulin, which helps regulate blood sugar. They also regulate how much sugar is released from the liver and slow down digestion.
Extensive preclinical studies and robust clinical trials have demonstrated the efficacy of GLP-1R agonists in both treating and preventing obesity. By mimicking the effects of our own GLP-1, these agents not only promote a feeling of fullness and reduce food intake but also enhance glucose balance. Given their multifaceted therapeutic benefits and favorable safety profile, GLP-1R agonists have emerged as particularly promising options for individuals struggling with obesity, offering a potential paradigm shift in medical weight management.1
Mechanisms Of Action
GLP-1RA medications employ multiple mechanisms to help with weight loss. These drugs mimic the glucagon-like peptide-1 hormone, which plays a vital role in blood sugar regulation and digestion. Their primary effects include reducing appetite and increasing calorie expenditure by activating brown fat tissue through the nervous system. Brown fat is the “fat-burning fat” that is able to burn off excess calories 24/7 as body heat. At the metabolic level, medications like liraglutide and semaglutide stimulate insulin production while decreasing sugar production in the liver. They also slow stomach emptying, making them valuable for supporting both type 2 diabetes and weight reduction. In addition, these medications regulate food intake through complex interactions with the gut-brain axis, influencing hunger-control centers in the brain and modulating the gut microbiome.2
Liraglutide and Semaglutide
Both medications are administered via injection, not oral pills. The injection pen, which comes pre-filled, makes it easy to set and deliver the correct dose. The injection sites are typically the abdomen, thigh, or upper arm.
The Good News
GLP-1RAs were initially designed for treating type 2 diabetes mellitus (T2DM), but they have demonstrated weight loss benefits in several clinical trials.3 Victoza (liraglutide) and Ozempic (semaglutide), have since been approved by the Food and Drug Administration as weight loss medications due to their effectiveness in promoting significant and sustained weight loss.4
New Study Reveals Many More Benefits
A new large-scale observational study analyzing Veterans Administration (VA) data from nearly 2 million military vets has revealed extensive insights into the effects of GLP-1 receptor agonists.5
New benefits that were revealed in this study include:
8% decrease in dementia risk
12% reduction in Alzheimer’s disease risk
Significant reductions in substance use disorders:
- Alcohol use (11% reduction)
- Cannabis use (12% reduction)
- Stimulant use (16% reduction)
- Opioid use (13% reduction)
10% reduction in suicide-related behaviors
19% reduction in schizophrenia and psychotic disorders
- 9% reduction in myocardial infarction
- 22% reduction in cardiac arrest
- 11% reduction in heart failure
- 7% reduction in ischemic stroke
- 14% reduction in hemorrhagic stroke
Reduced risks of pneumonia, COPD, and respiratory failure
12% reduction in bacterial infections
12% decrease in acute kidney injury
3% reduction in chronic kidney disease
Decreased risks of liver cancer and inflammatory bowel disease
Obesity increases the risk of major chronic diseases, so when an obese patient loses weight they also reduce their risk of cardiovascular disease, cancer, neurological diseases, arthritis, etc. Recent studies have highlighted long-term benefits associated with weight loss from taking GLP-1RAs,6 including a marked reduction in cardiovascular events, heart failure, and kidney disease.
The Bad: Side Effects and Muscle Loss
First off, despite substantial weight loss, many patients find staying on the medications difficult because of a lengthy list of uncomfortable side effects including: nausea, vomiting, constipation, gastroparesis, dehydration, acid reflux, low blood pressure, and gallstones.7
Secondly, a new study published in the July 2024 journal Gastroenterology,8 found that GLP-1s can increase the risk of pulmonary aspiration when a patient is under deep sedation during surgery. This can cause aspiration pneumonia, a lung infection that occurs when food or liquid is inhaled into the lungs. It appears that routine fasting before a surgery doesn’t seem to be enough, so it’s suggested that patients stop these medications at least 1 week prior to surgery.
Recent studies have shown that weight loss with GLP-1RA injections and combination therapies is approaching magnitudes achieved with bariatric surgery. However, as more weight loss is achieved, there is concern for potential adverse effects on muscle quantity, composition, and function. Factors such as older age and pre-frailty may influence the selection of appropriate candidates for these therapies because of risk for sarcopenia (muscle loss).9
A commentary published in the November issue of The Lancet10 by an international team of researchers examined emerging research showing that up to 40% of the weight lost by people using these drugs is actually muscle weight.
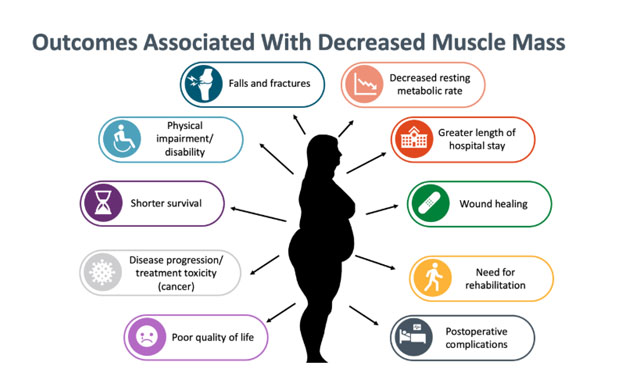
This graphic shows selected consequences of low muscle mass (or related conditions, such as sarcopenia, frailty, and cachexia) and malnutrition across aging and clinical populations11
Thyroid Cancer Risk
According to Dr. Varney, an assistant professor at the University of Virginia, thyroid cancer risks from GLP-1 weight loss medications mainly affect people with specific genetic conditions: multiple endocrine neoplasia 2 (MEN2) or medullary thyroid cancer (MTC). MTC is rare, accounting for only 3-5% of thyroid cancers.
The cancer risk depends on dosage. Animal studies used doses 8-60 times higher than human prescriptions, though some cases of thyroid cancer have been reported in humans taking these medications.12
A large study of over 350,000 type 2 diabetes patients found that GLP-1 receptor agonist users showed higher thyroid cancer rates in the first year of treatment compared to users of other diabetes medications (HR 1.85, 95% CI 1.11-3.08). However, researchers conclude this increase may likely stem from heightened surveillance rather than actual cancer development.13
Pancreatitis and Gallbladder Concerns
When prescribing these medications, doctors must consider a patient’s history of pancreatic inflammation (pancreatitis). These drugs have been found to increase the risk of acute pancreatitis by 2.5 %. While a family history of pancreatic cysts or cancer doesn’t prevent using these medications, they can increase gallbladder problems. Research from 202214 shows higher risks of gallbladder disease, especially with higher doses and longer use.
These medications may not be suitable for patients with:
- Slow stomach emptying (gastroparesis)
- Eye problems from diabetes
- Severe constipation
- Serious heartburn.15
The Ugly – When You Stop, You Not Only Gain the Weight Back, But You Usually Gain Back Even More
An important consideration is what happens when people stop taking these medications: even if they maintain a healthy diet and exercise habits, most people regain the weight they lost.
Researchers have known for a long time that there has been a noticeable trend of quick weight regain following the discontinuation of semaglutide and other GLP-1 RAs, as detailed in various trials.16
During weight loss, several biological changes compensate for and prevent the maintenance of long-term weight loss, and weight regain is commonly observed.17
Research has found several reasons for this weight regain after stopping the medication. These include changes in brain signaling, reduced hormone production, and the body’s natural tendency to adapt to weight loss by trying to return to its previous weight.18
Mechanisms Involved In Weight Gain After Stopping GLP-1RAs
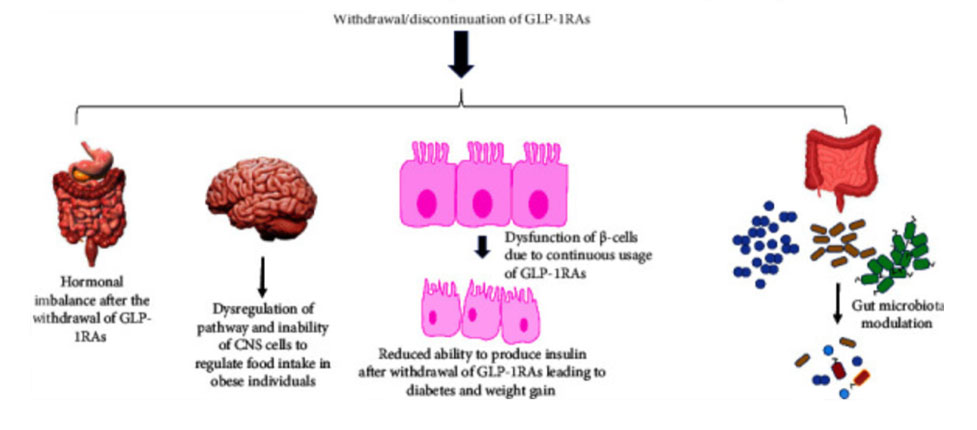
Copyright © 2024 Ibrahim Abdullah bin Ahmed.
If using these hormones, I think it’s really important from the get go, that people begin working with the Mederi Care approach to health optimization and healthy weight management.
“Out of your vulnerabilities will come your strength.”
– Sigmund Freud, neurologist and founder of psychoanalysis
What Every Patient Should Know If Considering GLP-1 RAs
Laura Davisson, MD, MPH, said, “Not every overweight patient is a good candidate for GLP-1 RAs, and it’s important that doctors explain why the medications may not be right for them…If a patient only has a few pounds to lose (15-20 lb) and does not accept that these medications are intended to be a long-term treatment for the chronic diseases of diabetes or obesity, then they might not be a good candidate for the medication.”
Also essential is making sure patients are willing to follow appropriate healthy eating guidelines when on the medications, including getting enough protein, veggies, and fruits to maintain lean mass, and enough fiber to keep bowel habits regular.
This class of medication has been used for nearly 20 years to treat type 2 diabetes, and the data over the past two decades have shown that the benefits of GLP-1 RAs far outweigh the risks for most patients.
I have written a wonderful chapter in my book, “Adaptogens in Medical Herbalism” on Weight management. Here are two previous blogs of mine that will also help with a truly holistic approach to weight management and being the best version of yourself.
- Six Targets For Optimal Weight Using Botanicals – https://www.donnieyance.com/six-targets-for-optimal-weight-using-botanicals/
- How To Be Healthy and Happy Achieving Your Optimal Weight https://www.donnieyance.com/how-to-be-healthy-and-happy-achieving-your-optimal-weight/
The Muscle Loss Tragedy
The crucial roles of skeletal muscle have come to the forefront of public attention due to data on the use of GLP-1 receptor agonists, which are effective for weight loss, but can cause substantial muscle loss.
Beyond its obvious role in movement and physical function, skeletal muscle serves as the body’s largest reservoir of amino acids, plays a vital role in metabolic health, and functions as an endocrine organ secreting various myokines that influence whole-body metabolism. Recent clinical evidence has demonstrated that maintaining adequate muscle mass is essential for healthy aging, improved chronic disease outcomes, and enhanced recovery from acute illness.
The emergence of popular weight loss medications like semaglutide and tirzepatide has highlighted the critical need to understand and preserve muscle mass during weight loss interventions, as the loss of muscle tissue could compromise these critical physiological functions.19
The first thing to keep in mind is that your body weight isn’t just about calories in and calories out. Sure, that’s part of the equation, but there’s a deeper story happening beneath the surface.
Nourishing Opportunities
Here’s a thought that might change how you look at your next meal: Every time you choose what to eat, you’re actually making two choices at once. It’s a fascinating way to think about food that goes beyond the usual “good versus bad” conversation.
Think of it this way – when you reach for a processed snack instead of something whole and natural, you’re not just consuming something that might harm your health. You’re also missing a golden opportunity to give your body something healing and nourishing. It’s like turning down natural medicine while taking something that makes you feel worse.
But here’s where we can flip the script. Instead of carrying around a mental list of foods to avoid (which, let’s face it, can be exhausting), what if we got excited about all the incredible foods we can eat? This isn’t just positive thinking – it’s a powerful way to transform your health.
Your grocery store’s produce section is really nature’s pharmacy in disguise. Those vibrant fruits and vegetables aren’t just pretty to look at – they’re packages of natural medicine. Each color, from deep purple berries to bright-green leafy vegetables, represents different compounds that can heal and protect your body.
When you start thinking this way, healthy eating becomes less about restriction and more about opportunity. Instead of asking “What should I avoid?” try asking “What healing foods can I add to this meal?”
This simple shift can transform eating from a source of stress into an act of self-care. The beauty of this approach is that when you focus on adding good things to your diet, the less healthy choices naturally get crowded out.
The Fast Food Factor
Our modern world has brought us convenience, but at what cost? Fast food, with its perfect storm of high calories, processed ingredients, and easy accessibility, has changed the way we eat. These foods don’t just add calories to our diet – they actually change how our bodies process energy. It’s like filling up your precision sports car engine with the wrong fuel.
The Hidden Players: Blood Sugar and Fat Metabolism; Here’s Where Things Get Really Interesting.
Two key players in this complex dance are:
- Blood Sugar (Hyperglycemia): When we consistently flood our bodies with high-calorie, processed foods, our blood sugar regulation system starts to falter. It’s like constantly revving a car engine – eventually, something’s got to give.
- Fat Processing (Dyslipidemia): Our bodies have an amazing ability to process and store fats, but modern diets can overwhelm this system. Think of it as trying to force too much traffic through a small street – eventually, everything backs up.
The complex web that makes obesity such a challenging issue is how these factors interact with each other. Your blood sugar levels affect your fat storage, which influences your energy levels, which impacts your activity, which circles back to affect your blood sugar… It’s a continuous cycle where each element influences the others.
Understanding this complexity is crucial because it helps us realize why the simple “eat less, move more” advice often falls short. It’s not just about willpower or counting calories – it’s about understanding and working with your body’s intricate systems.
A better approach- instead of focusing solely on calories, consider:
- The quality of your food choices
- How different foods affect your blood sugar
- The timing of your meals
- Your body’s unique way of processing nutrients.20
Obesity is associated with a wide range of metabolic dysfunctions, which affect multiple organs of the body and subsequently disrupt their regular function.
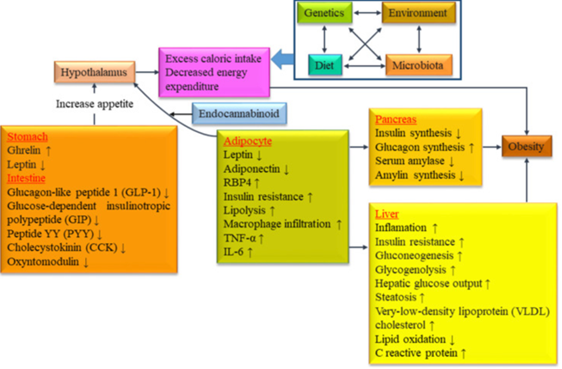
Interconnection between genetic factors, environmental factors, dietary patterns and gut microbiota associated with the incidence of obesity.21
Instead of falling for quick fixes or extreme diets, we can work with our bodies’ natural systems to find balance and health. Remember, your body is incredibly complex and wonderful. By understanding and respecting this complexity, we can make more informed choices about our health and well-being. One of the basic concepts and directives of the Unitive System, called Mederi Care, is to enhance anabolic metabolism, efficiency, and auto-regulation at the molecular, cellular, and organ system levels.
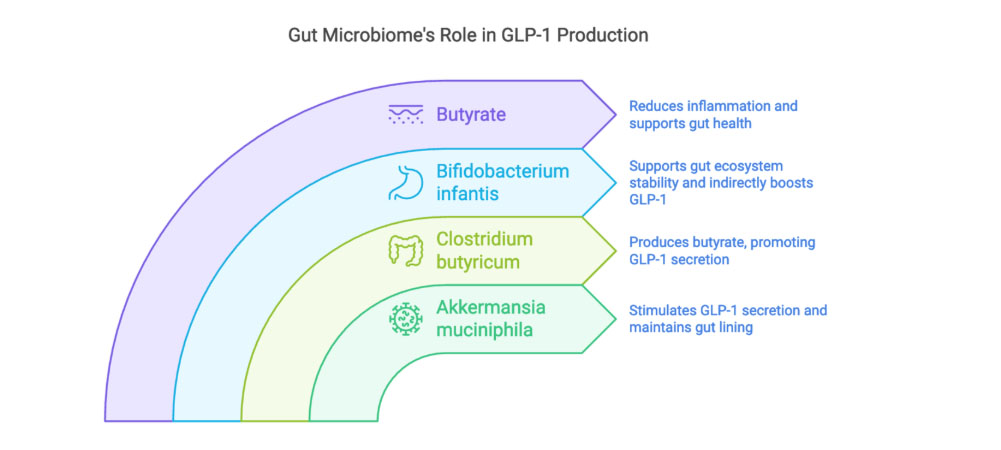
The Intricate Relationship Between Gut Health and GLP-1
One of the most exciting insights into GLP-1 is the role of the gut microbiome in its production. Research has identified specific beneficial bacteria that play crucial roles in GLP-1 secretion and overall metabolic health. These microorganisms work through complex mechanisms, primarily through the production of short-chain fatty acids (SCFAs), to influence our body’s GLP-1 levels.
Key Bacterial Players in GLP-1 Production
Several beneficial bacteria have emerged as important contributors to GLP-1 regulation:
- Akkermansia muciniphila: This beneficial bacteria stimulates GLP-1 secretion while maintaining gut lining integrity. Research shows that individuals with higher Akkermansia levels typically demonstrate better metabolic health markers and lower obesity risk.
- Clostridium butyricum: Known for its production of butyrate, a vital SCFA that promotes GLP-1 secretion. Butyrate’s benefits extend beyond GLP-1, including reduced inflammation and enhanced gut barrier function.
- Bifidobacterium infantis: While indirectly affecting GLP-1, this bacteria produces essential metabolites that support other beneficial bacteria, helping maintain a balanced gut ecosystem.
Dietary Interventions to Optimize GLP-1 Levels
A diet rich in specific nutrients can naturally enhance GLP-1 production through the gut microbiome:
- Fiber-Rich Foods: Include plenty of vegetables, fruits, potatoes, and whole grains
- Polyphenol Sources: Incorporate berries, leafy greens, and nuts
- Probiotic-Rich Foods: Add fermented foods to support beneficial bacteria
Anabolic – Catabolic and Metabolic Optimization
An adequate balance between catabolic (mobilization of energy) and anabolic processes (growth & healing) is considered necessary for long-term health and survival. In modern society, which is characterized by a rapid pace of life, high demands, efficiency, and competitiveness, it is likely that a lack of rest and recovery is a greater health problem than the absolute level of stress.
Anabolic-Inward ‘yin’ Energy and Catabolic-outward ‘yang’ Energy
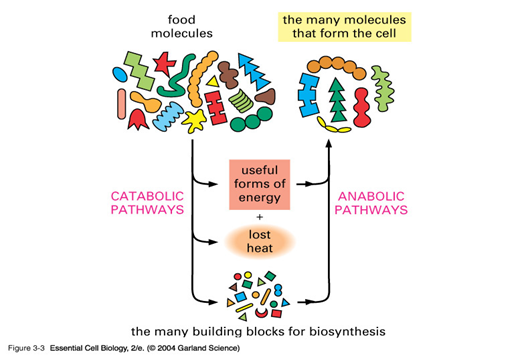
Foods we eat are either used to produce energy, which is a catabolic process, or to build and repair cells, which is an anabolic process. Foods of plant origin contain many hundreds of compounds which cannot be considered as nutrients, but appear to play a role in the maintenance of health. Whole foods and herbs contain a symphony of phytonutrients including: flavonoids, terpenoids, lignans, sulfides, polyphenolics, carotenoids, coumarins, saponins, plant sterols, and phthalides; these have been researched and found to possess important actions in health promotion and disease prevention.
Recent research in this area indicates that the impact of a number of diseases affecting humans and animals can be prevented or reduced by 50% or more through dietary and supplemental intake of these amazing plant molecules.
22
The field of nutrigenomics is the use of genomic tools to study diet-gene interactions and identify food components that have beneficial or detrimental effects. Nutrition is truly one of the environmental factors influencing gene expression.
The interplay, communication, and synergy between nutrient-dense foods and herbs is now scientifically demonstrating nothing short of a deep and beautiful ‘love’ whereby our cells take up these phytonutrients and build healthy strong cells able to perform magnificently.
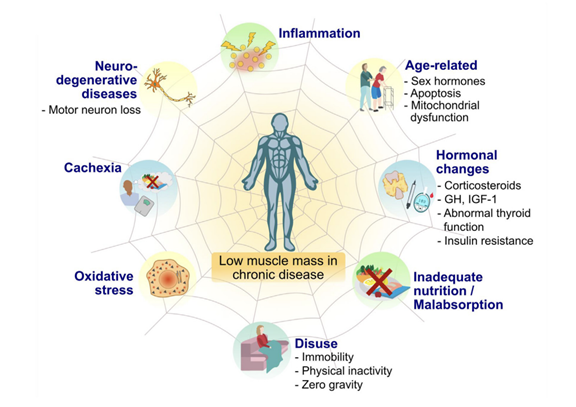
Selected risk factors that contribute to low muscle mass in people with chronic conditions. Abnormalities in muscle mass can emerge if at least one of these factors is present; however, multiple risk factors in chronic disease can lead to severe low muscle mass. Abbreviation: GH, growth hormone; IGF-1, insulin-like growth factor 1.23
Protein and Immune Health
Adequate intake of high-quality absorbable protein is essential for optimal immune response and for enhancing lean muscle mass. Since antibodies are protein structures, low protein intake or utilization can lead to low antibody production or a poor immune response.
Metabolism and Aging
A decline in protein synthesis (decreased anabolic activity) is the single most important indication of aging. As muscle mass diminishes, muscle strength begins its downfall. This catabolic process also results in decreased muscle strength, heart health, bone density, obesity, impaired glucose metabolism, accelerated aging, and reduction in quality of life.
Anabolic restoration with diet, exercise, rest, and botanical-nutritional formulations, is the core to my approach to health promotion, disease prevention, and healthy aging.
The importance of enhancing cellular protein synthesis cannot be overstated. Aging causes a decline in protein synthesis that inevitably leads to disability and death.
It is the single most overlooked and under-treated key factor to health that there is.
Boosting Protein Synthesis
Scientists have found that administering: amino acids, creatine, Hydroxymethylbutyrate (HMB), and glutamine, with cofactors such as boron, chromium, and vanadium, increased net muscle protein synthesis by increasing amino acid transport into muscle cells.
Other anabolic-immunonutrients include the amino acids L-arginine, L-citrulline, and carnitine. This combination increased amino acid delivery to the cells, stimulated muscle protein synthesis, and prevented weakness throughout the body. This anabolic response achieved with amino acids and botanical compounds shows that muscle mass can be preserved and restored.
Conclusion
To sum up, while GLP-1 receptor agonists like semaglutide and liraglutide offer promising options for diabetes and weight loss, they are not without risks and side effects. The potential for muscle loss, GI symptoms, cardiac effects, and weight regain after stopping use highlights the importance of a holistic approach to health. Combining these medications with balanced nutrition, adequate protein intake, and sustainable lifestyle changes can help preserve muscle mass, optimize metabolic function, and support long-term health.
As with any medical treatment, individualized care and informed decision-making are essential to achieving the best outcomes. It is best to work with a knowledgeable holistic provider along with your prescribing doctor to determine the best approach for your unique health needs and goals.
In Part 2, we will go more in depth on the specific nutrients and steps that you can take to optimize your health and weight loss journey if you and your doctor decide that these GLP-1 receptor agonists are right for you.
About the Author:
Donald R. Yance is the founder of the Mederi Center. A Clinical Master Herbalist and Certified Nutritionist, Donnie is renowned for his extraordinary knowledge and deep understanding of the healing properties of plants and nutrition, as well as of epigenetics, laboratory medicine, oncologic pathology, and molecular oncology. He is a professional member of the American Herbalists Guild, National Association of Nutrition Professionals, Academy of Integrative Health and Medicine, and the Society for Integrative Oncology.
References:
1 Wang JY, Wang QW, Yang XY, Yang W, Li DR, Jin JY, Zhang HC, Zhang XF. GLP-1 receptor agonists for the treatment of obesity: Role as a promising approach. Front Endocrinol (Lausanne). 2023 Feb 1;14:1085799. doi: 10.3389/fendo.2023.1085799.
2 Wang J. Y., Wang Q.-W., Yang X.-Y., et al. GLP-1 receptor agonists for the treatment of obesity: role as a promising approach. Frontiers in Endocrinology . 2023;14 doi: 10.3389/fendo.2023.1085799.1085799
3 Abdullah Bin Ahmed I. A Comprehensive Review on Weight Gain following Discontinuation of Glucagon-Like Peptide-1 Receptor Agonists for Obesity. J Obes. 2024 May 10;2024:8056440. doi: 10.1155/2024/8056440. PMID: 38765635; PMCID: PMC11101251.
4 Raza FA, Altaf R, Bashir T, Asghar F, Altaf R, Tousif S, Goyal A, Mohammed A, Mohammad MF, Anan M, Ali S. Effect of GLP-1 receptor agonists on weight and cardiovascular outcomes: A review. Medicine (Baltimore). 2024 Nov 1;103(44):e40364. doi: 10.1097/MD.0000000000040364. PMID: 39496023; PMCID: PMC11537668.
5 Xie Y, et al “Mapping the effectiveness and risks of GLP-1 receptor agonists”; Nat Med 2025; DOI: 10.1038/s41591-024-03412-w.
6 Ussher, J.R., Drucker, D.J. Glucagon-like peptide 1 receptor agonists: cardiovascular benefits and mechanisms of action. Nat Rev Cardiol 20, 463–474 (2023). https://doi.org/10.1038/s41569-023-00849-3
7 Expert Tips for Managing GLP-1 Medication Side Effects - Medscape - December 27, 2024.
8 Yeo, Yee HuiGaddam, SrinivasNg, Wee HanHuang, Pin-ChiaMohamed, GhadaMa, Kevin Sheng-KaiRezaie, Ali et al. Increased Risk of Aspiration Pneumonia Associated With Endoscopic Procedures Among Patients With Glucagon-like Peptide 1 Receptor Agonist Use Gastroenterology, Volume 167, Issue 2, 402 – 404.e3
9 Linge J, Birkenfeld AL, Neeland IJ. Muscle Mass and Glucagon-Like Peptide-1 Receptor Agonists: Adaptive or Maladaptive Response to Weight Loss? Circulation. 2024 Oct 15;150(16):1288-1298. doi: 10.1161/CIRCULATIONAHA.124.067676. Epub 2024 Oct 14. PMID: 39401279.
10 Carla M Prado et al, Muscle matters: the effects of medically induced weight loss on skeletal muscle, The Lancet Diabetes & Endocrinology (2024). DOI: 10.1016/S2213-8587(24)00272-9
11 Clinicaloptions.com, Prado CM, Landi F, Chew STH, Atherton PJ, Molinger J, Ruck T, Gonzalez MC. Advances in muscle health and nutrition: A toolkit for healthcare professionals. Clin Nutr. 2022 Oct;41(10):2244-2263. doi: 10.1016/j.clnu.2022.07.041. Epub 2022 Aug 7. PMID: 36081299.
12 Should Patients With Thyroid Issues Take GLP-1s? It Depends - Medscape - December 19, 2024.
13 Brito JP, et al “GLP-1RA use and thyroid cancer risk” JAMA Otolaryngol Head Neck Surg 2025; DOI: 10.1001/jamaoto.2024.4852.
14 He L, Wang J, Ping F, et al. Association of Glucagon-Like Peptide-1 Receptor Agonist Use With Risk of Gallbladder and Biliary Diseases: A Systematic Review and Meta-analysis of Randomized Clinical Trials. JAMA Intern Med. 2022;182(5):513–519. doi:10.1001/jamainternmed.2022.0338
15 Sodhi M, Rezaeianzadeh R, Kezouh A, Etminan M. Risk of Gastrointestinal Adverse Events Associated With Glucagon-Like Peptide-1 Receptor Agonists for Weight Loss. JAMA. 2023;330(18):1795–1797. doi:10.1001/jama.2023.19574
16 Sjöström L., Rissanen A., Andersen T., et al. Randomised placebo-controlled trial of orlistat for weight loss and prevention of weight regain in obese patients. The Lancet . 1998;352(9123):167–172. doi: 10.1016/s0140-6736(97)11509-4.
17 (PDF) A Comprehensive Review on Weight Gain following Discontinuation of Glucagon-Like Peptide-1 Receptor Agonists for Obesity. Available from: https://www.researchgate.net/publication/380516821_A_Comprehensive_Review_on_Weight_Gain_following_Discontinuation_of_Glucagon-Like_Peptide-1_Receptor_Agonists_for_Obesity [accessed Nov 27 2024].
18 Lopez-Jimenez F., Almahmeed W., Bays H., et al. Obesity and cardiovascular disease: mechanistic insights and management strategies. A joint position paper by the World Heart Federation and World Obesity Federation. European Journal of Preventive Cardiology . 2022;29(17):2218–2237. doi: 10.1093/eurjpc/zwac187.
19 Paschalis Karakasis, Dimitrios Patoulias, Nikolaos Fragakis, Christos S. Mantzoros, Effect of glucagon-like peptide-1 receptor agonists and co-agonists on body composition: Systematic review and network meta-analysis, Metabolism, 164, (156113), (2025).
20 Abdisa KB, Szerdahelyi E, Molnár MA, Friedrich L, Lakner Z, Koris A, Toth A, Nath A. Metabolic Syndrome and Biotherapeutic Activity of Dairy (Cow and Buffalo) Milk Proteins and Peptides: Fast Food-Induced Obesity Perspective-A Narrative Review. Biomolecules. 2024 Apr 14;14(4):478. doi: 10.3390/biom14040478.
21 Abdisa KB, Szerdahelyi E, Molnár MA, Friedrich L, Lakner Z, Koris A, Toth A, Nath A. Metabolic Syndrome and Biotherapeutic Activity of Dairy (Cow and Buffalo) Milk Proteins and Peptides: Fast Food-Induced Obesity Perspective-A Narrative Review. Biomolecules. 2024 Apr 14;14(4):478. doi: 10.3390/biom14040478. (self-developed, concept was adopted from Ussar et al., 2016
22 https://courses.lumenlearning.com/suny-ap2/chapter/overview-of-metabolic-reactions/
23 Prado CM, Landi F, Chew STH, Atherton PJ, Molinger J, Ruck T, Gonzalez MC. Advances in muscle health and nutrition: A toolkit for healthcare professionals. Clin Nutr. 2022 Oct;41(10):2244-2263. doi: 10.1016/j.clnu.2022.07.041. Epub 2022 Aug 7. PMID: 36081299.

